Knee
ACL (Anterior Cruciate Ligament) Injury
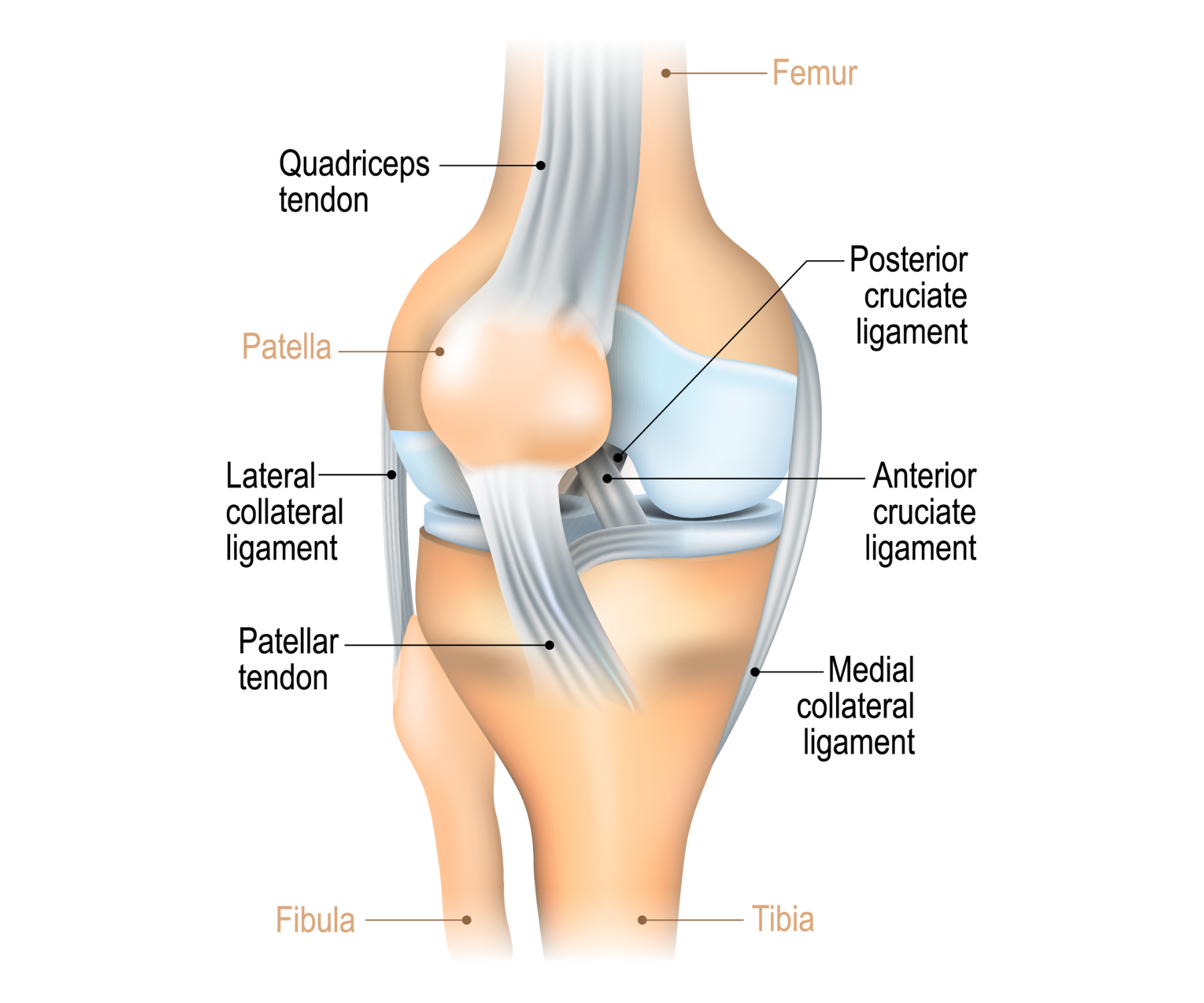
The anterior cruciate ligament (ACL) is one of the most critical structures in the knee joint, which prevents anterior translation of the tibia in relation to the femur and also offers rotational stability.
ACL injuries are one of the most prevalent orthopedic issues, specifically in young athletes involved in sports such as football, basketball, soccer, and skiing.
A tear in the ACL can happen due to a non-contact mechanism—most likely when the athlete suddenly changes direction, lands awkwardly, or quickly decelerates.Or, contact injuries through collisions or falls. Patients typically describe a popping sensation at injury, along with immediate swelling, knee instability, and weight-bearing difficulty. The disorder can result in long-term instability, meniscal tears, cartilage loss, and premature osteoarthritis if left untreated. MRI is the diagnostic gold standard, with clinical tests like the Lachman and pivot shift tests giving severe indications of instability.
Causes:
- Non-contact pivoting on a planted foot with a hyperextended knee.
- Inadequate neuromuscular control in muscle imbalance athletes.
- Direct trauma during contact sports due to hyperextension or rotational stress.
- Sudden deceleration or direction change, particularly on an unstable surface.
- Valueless landing biomechanics—valgus collapse of the knee and absence of hip control.
Prevention:
- Prevention of ACL injuries is possible through preventive measures aimed at neuromuscular control, strength, and balance. Good programs include:
- Individual neuromuscular training with plyometrics, balance exercises, and proprioception.
- Hamstring, glute, and core strengthening to minimize stress on the ACL.
- Proper landing mechanics training and prevention of valgus knee positioning.
- Cleat or proper footwear for the playing surface.
- Fatigue management with sufficient rest and recovery between practice sessions.
Advantages of Treatment:
- Treatment depends on the patient’s lifestyle, age, and degree of injury. Partial tears may be managed conservatively, but complete tears, especially in active individuals, often require surgical intervention.
- ACL reconstruction using autografts (hamstring, patellar, or quadriceps tendon) restores knee stability and function.
- Advanced surgical techniques like anatomical double-bundle reconstruction better mimic native ligament biomechanics.
- Rehabilitation post-surgery involves 6–12 months of progressive strength and proprioceptive training.
- PRP or BMAC therapy may be employed adjunctively to improve graft integration and decrease inflammation.
- Well-managed ACL injuries permit return to sport, maintain long-term knee function, and decrease risk of subsequent joint deterioration.
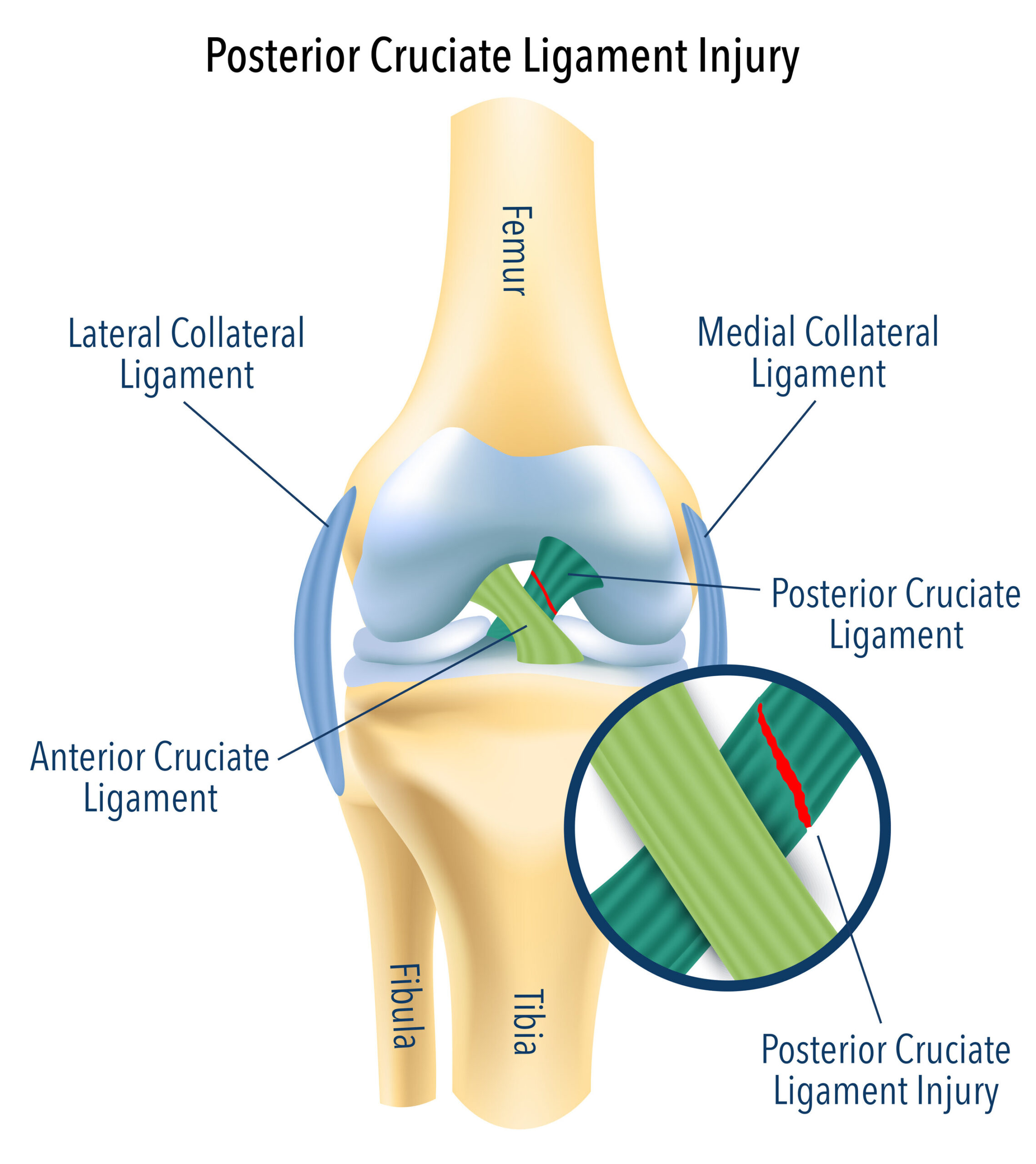
PCL (Posterior Cruciate Ligament) Injury
The posterior cruciate ligament (PCL) is the major restraint against posterior tibial displacement.
It is wider and denser than the ACL and therefore injured less often, but tears of the PCL are functionally disabling.The PCL supports the knee during activities like walking down a hill, descending stairs, and landing after a jump.Injuries usually result from a direct impact to the tibia as the knee is flexed, e.g., from a car accident (dashboard type) or falling over the front of the knee.Isolated PCL injuries can be less symptomatic at first, but chronic instability, abnormal gait, patellofemoral pain, and premature osteoarthritis may result if it is not treated. Diagnosis is posterior drawer testing, tibial sag sign, and MRI confirmation.
Causes:
- Dashboard impact during a car crash that forces the tibia backward.
- Landing on a flexed knee with sports or activities such as hiking or skating.
- Hyperflexion or hyperextension injury.
- Tackling or landing on the knee sports such as football.
Prevention:
- PCL injury prevention is based on general knee strength and dynamic control:
- Specific quadriceps strengthening to counteract posterior tibial motion.
- Avoiding high-risk behaviors without equipment (e.g., skateboarding with pads).
- Agility and proprioceptive drills for neuromuscular coordination.
- Safe deceleration, jumping, and landing mechanics instruction.
Advantages of Treatment:
- Most PCL injuries can be effectively treated nonoperatively, particularly isolated Grade I or II ruptures.
- Functional bracing and organized rehab reestablishes stability and strength.
- Surgery is advised for high-grade ruptures, avulsions, or multiligament sprains.
- PCL reconstruction with autografts or allografts can restore full function of the joint.
- Postoperative rehabilitation enhances the stability of the posterior knee and limits long-term degeneration.
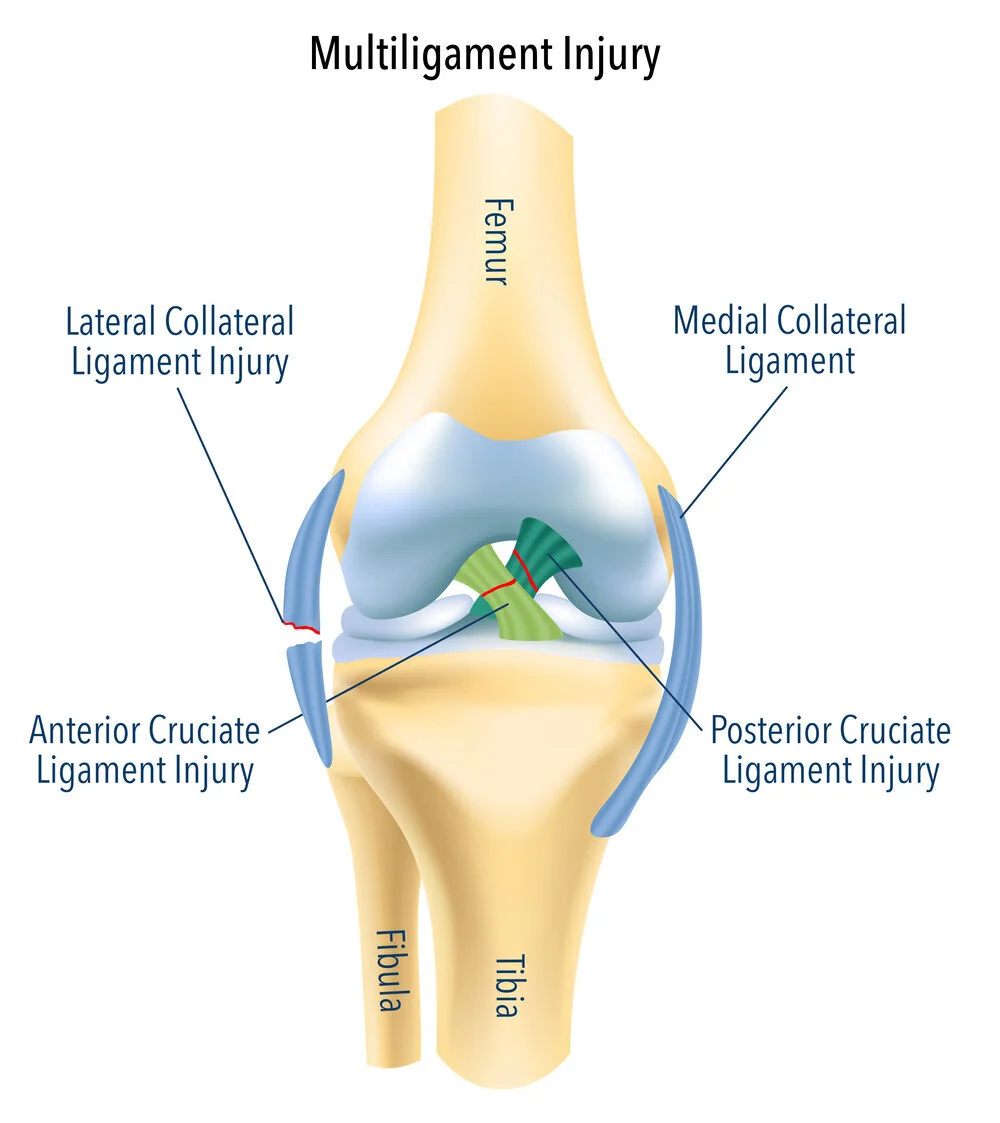
Multiligament Knee Injury:
Multiligament knee injuries (MLKIs) are severe and often traumatic injuries involving two or more of the major stabilizing ligaments of the knee: ACL, PCL, MCL, and LCL.
Capsule, meniscus, cartilage, and neurovascular structures may be affected with these injuries.
High-energy trauma involves MLKIs with the possible mechanism being motor vehicle accidents or falls from a height.
The knee is grossly unstable, and complications such as popliteal artery or peroneal nerve injury are likely. MLKIs usually necessitate multiple staged operations and prolonged rehabilitation.Clinical testing, imaging, and vascular evaluation (e.g., Doppler ultrasound or CT angiogram) are necessary for proper diagnosis and planning.
Causes:
- High-impact motor vehicle trauma.
- Falls of large stature with twisting forces.
- Sports injuries with violent hyperextension or valgus/varus stress.
- Industrial injuries or crush.
Prevention:
- Wearing protective equipment during thrill sports or manual labor work.
- Early treatment of isolated ligament sprains to avoid aggravation.
- Core, hip, and knee strengthening to increase joint stability.
- Early recognition of high-risk activities or settings.
Advantages of Treatment:
- Well-organized and timely treatment is essential:
- Acute stabilization minimizes soft tissue damage and neurovascular compromise.
- Multiligament reconstruction restores functional anatomy and load balance.
- Arthroscopic and open surgical methods are employed based on the level of injury.
- Postoperative rehabilitation is tailored, starting with protection, then progressively loading.
- Restored joint function allows return to work or adapted sporting activity.
Meniscus Tears:
The medial and lateral menisci are fibrocartilaginous structures that absorb and support the knee by dispersing axial loads and minimizing friction between the tibia and femur.
Tears result from acute trauma or chronic wear and tear, in athletes and elderly persons.
Mechanisms of injury are twisting, pivoting, or impact under weight-bearing.
Symptoms are joint line pain, effusion, catching, clicking, and locking of the knee.
Tears are categorized by morphology (e.g., radial, horizontal, bucket-handle), and treatment depends on vascular zone involvement.MRI is imaging of choice, and arthroscopy is both diagnostic and therapeutic
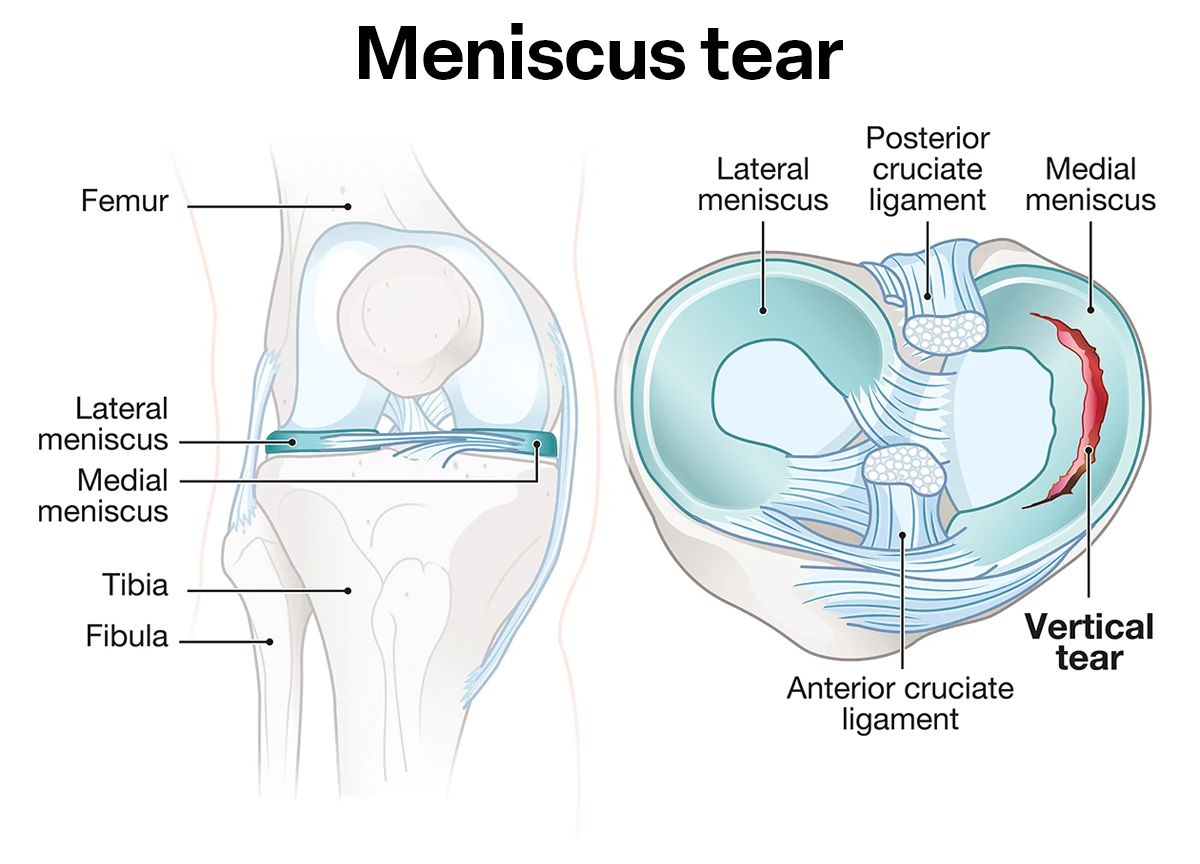
Causes:
- Wear supportive shoes for the knees and eschew high-risk sports without conditioning.
- Training balance and functional strengthening to aid joint control.
- Pivoting or twisting when playing sports such as soccer, basketball, or skiing.
Deep knee bending or squatting with work or heavy lifting. Cartilage degeneration due to age, especially in individuals above 40. - Traumatic knee injuries with ligamentous injuries. Prevention: Keep the quadriceps and hamstring muscles strong.
- Shun deep squats and rotation with faulty alignment.
Advantages of Treatment:
- Peripherally located tears can be cured with conservative treatments such as rest, NSAIDs, and physical therapy.
- Meniscal repair maintains long-term knee function and joint space.
- Arthroscopic partial meniscectomy can alleviate symptoms in non-reparable tears.
- PRP or BMAC can improve meniscal healing, particularly in borderline lesions.
- Early treatment prevents early arthritis, especially in active patients.
