Ankle
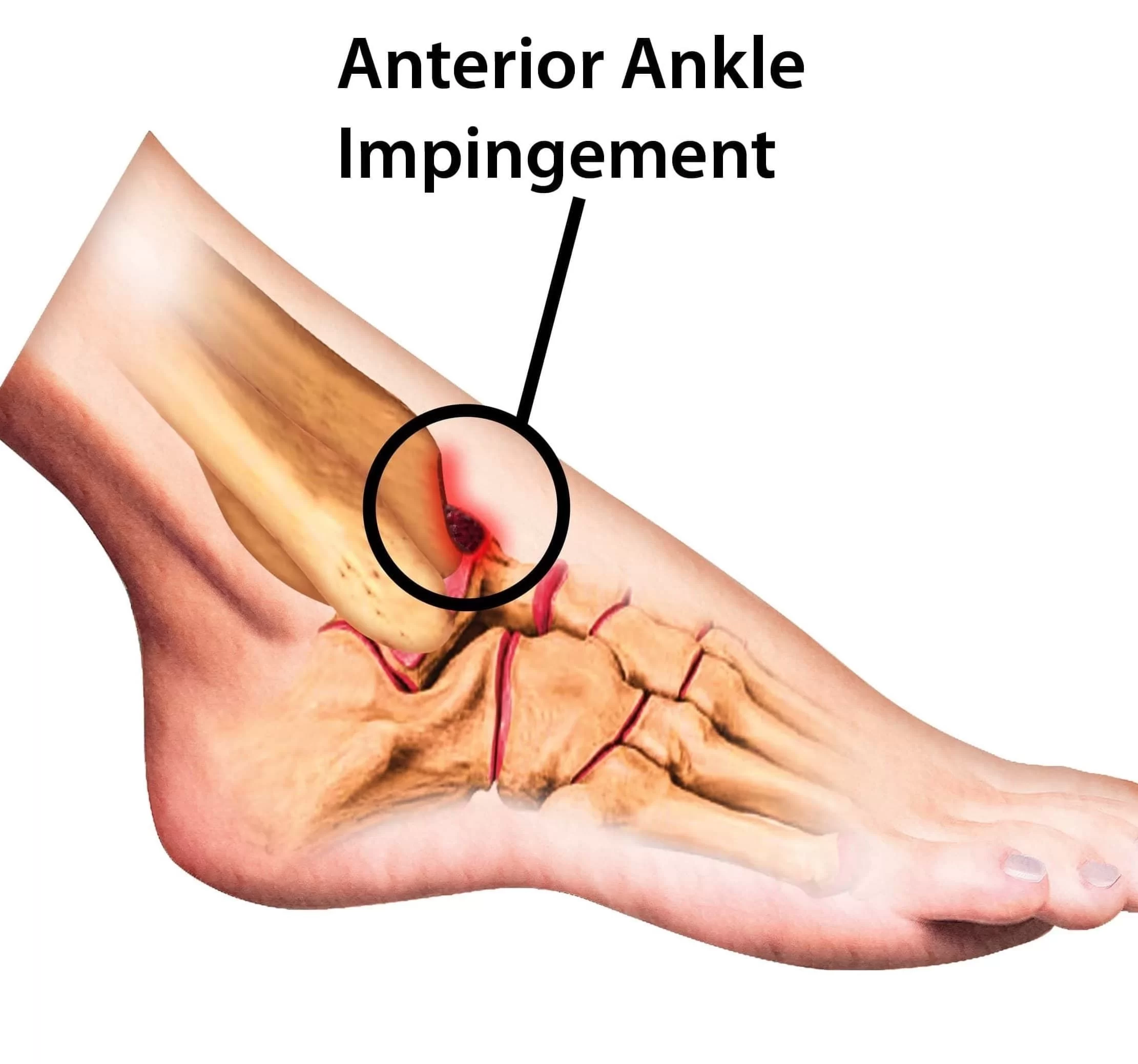
Ankle Impingement
Ankle impingement is a symptomatic condition in which soft structures or bony elements are pinched upon ankle motion, resulting in chronic inflammation, limited range of motion, and swelling.It is generally divided into anterior or posterior impingement.Anterior ankle impingement is when tissues at the front of the ankle joint are compressed in dorsiflexion (i.e., when squatting or walking uphill), while posterior impingement occurs at the back of the ankle in plantarflexion (i.e., when pointing one’s toes, a frequent movement for dancers).
This condition especially occurs in athletes who do repetitive movement on the ankle, such as footballers, ballet dancers, runners, or have a history of sprained ankle.
Bony spurs, scar tissues, or thickened ligaments contributed to this by decreasing joint space, hence not enabling movement.If not treated, ankle impingement may cause chronic pain, instability, and degenerative joint changes.
Causes:
- Repetitive dorsiflexion or plantarflexion of the ankle (e.g., dancing, soccer, or running).
- History of ankle sprains resulting in scar tissue formation or ligament thickening.
- Bone spur formation (osteophytes) from repetitive joint loading or trauma.
- Soft tissue entrapment such as thickened synovium or inflamed joint capsule.
Prevention:
- Avoid overtraining and include adequate rest periods in sports involving repetitive ankle movement.
- Perform regular ankle mobility and flexibility exercises to prevent stiffness.
- Strengthen surrounding muscles (calves, peroneals, tibialis anterior) to support ankle mechanics.
- Wear appropriate shoes with support and cushioning specific to the activity.
Advantages of Treatment:
- Conservative treatment with rest, NSAIDs, physical therapy, and taping usually resolves symptoms.
- Specific physiotherapy enhances joint mechanics, soft tissue mobility, and proprioception.
- Corticosteroid injection or regenerative treatments such as PRP can decrease inflammation in chronic cases.
- Surgical arthroscopic debridement excises bony spurs or scar tissue, easing mechanical block.
- Patients are able to return to full activity with enhanced ankle motion and decreased pain.
Treatment Option:
- Arthroscopic Debridement: Removal of bone spurs, hypertrophic synovium, or scar tissue from anterior or posterior ankle compartment.
- Open Surgery (in chronic impingement): Resection of osseous blocks if large or inaccessible arthroscopically.
OCD (Osteochondritis Dissecans) of the Ankle:
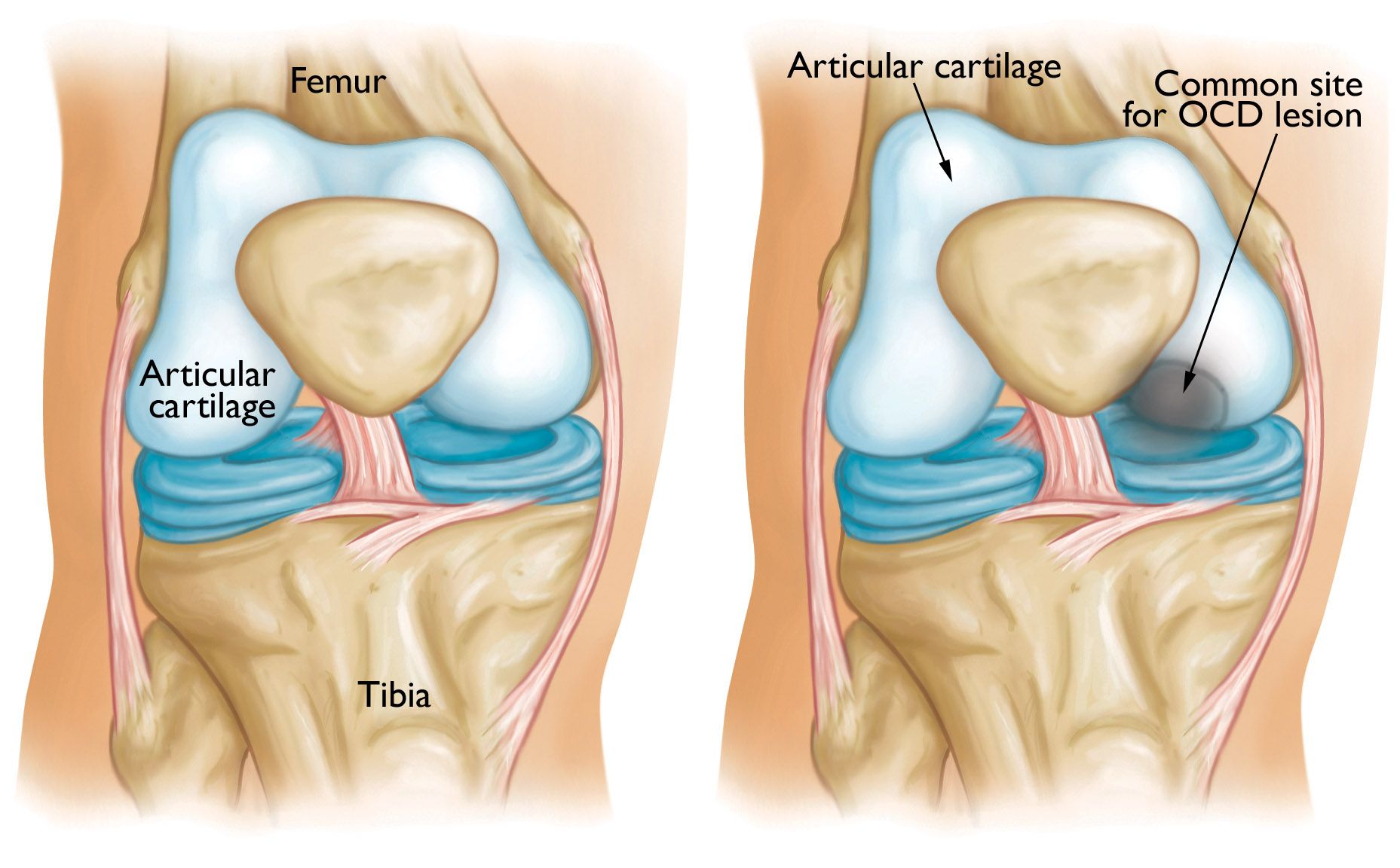
Osteochondritis dissecans (OCD) of the ankle is an injury in which a piece of bone and cartilage are damaged and can separate from the talar dome as a result of impaired blood supply.
This results in pain, swelling, stiffness of the joint, and locking or catching of the ankle joint.
OCD is most frequently seen in adolescent athletes and young adolescents, especially following ankle trauma such as sprain or chronic microtrauma.Lesions are classified as stable (intact) or unstable (loose fragments), which determines the need for surgery.MRI and CT scans help assess the depth, location, and stability of the lesion.If untreated, OCD can result in cartilage degeneration and early ankle arthritis.
Causes:
- Repeated ankle sprains or trauma resulting in shear force across the talar dome.
- Microtrauma from sports like basketball, gymnastics, or running.
- Interruption of blood flow (avascular necrosis) resulting in subchondral bone loss.
Prevention:
- Early treatment of ankle sprains to prevent recurrent joint laxity.
- Annual orthopedic examination in athletes with high training volumes.
- Cross-training and low-impact activities to minimize repetitive joint stress. Properly supported arch and ankle footwear.
Advantages of Treatment:
- Stable lesions usually heal with rest, immobilization, and physical therapy.
- Surgical options like drilling (microfracture), fixation, or osteochondral grafting restore joint integrity.
- Advanced biologic options like BMAC or PRP may enhance healing of subchondral bone and cartilage.
- Timely treatment prevents further joint surface erosion and arthritis progression.
- Most patients return to sports within 4–6 months post-treatment.
Treatment Option:
- Osteochondral Drilling, Microfracture, or Grafting: Based on lesion size and depth.
- May include autologous chondrocyte implantation or osteochondral autograft transfer (OATS).
Ankle Ligament Injuries:
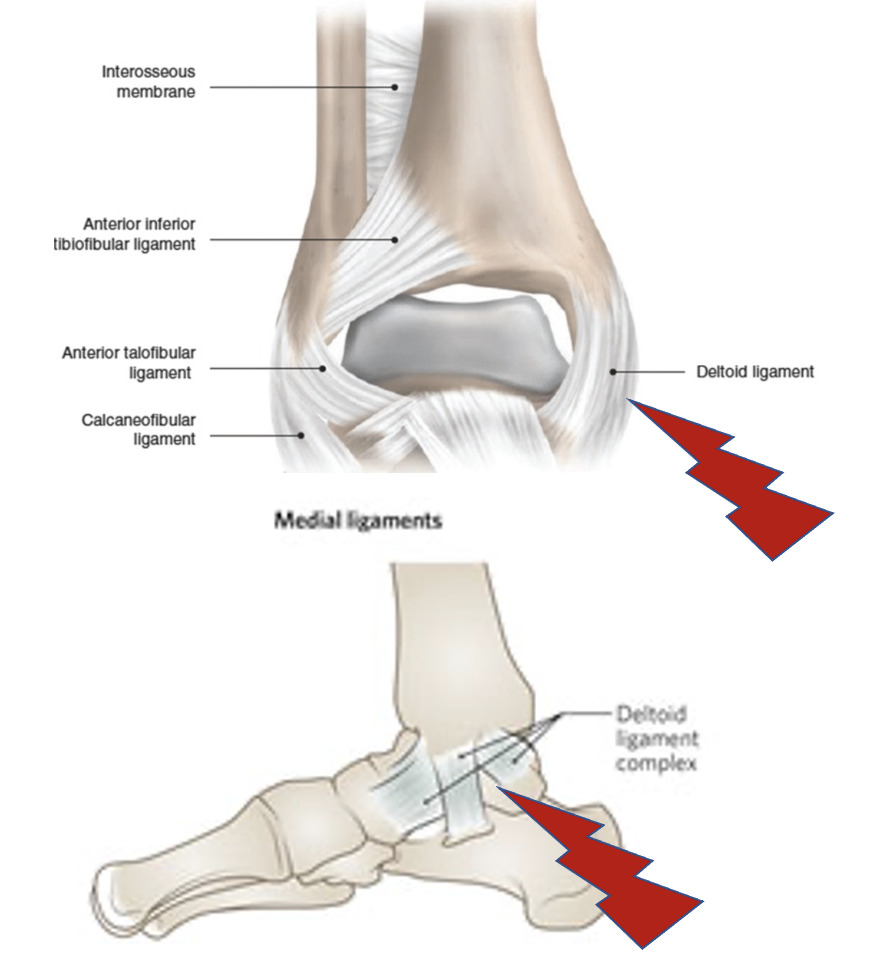
Ankle ligament injuries are among the most common musculoskeletal injuries, especially in sports and active populations. These injuries occur when the ligaments supporting the ankle joint are stretched beyond their limit or torn.The lateral ligaments (especially the anterior talofibular ligament or ATFL) are most commonly affected during an inversion injury (foot turning inward).Medial (deltoid) and high ankle sprains (syndesmotic injuries) may also occur but are less frequent.Ligament injuries are categorized as Grade I (mild), Grade II (partial tear), or Grade III (complete tear).Symptoms usually consist of swelling, bruising, weight-bearing pain, and instability.If not properly managed, recurrent sprains can culminate in chronic ankle instability and permanent disability.
Causes:
- Turning or twisting the ankle playing sports or walking on rough surfaces.
- Recurrent ankle sprains reduce ligament strength.
- Poor shoes, particularly high heels or flimsy sneakers.
- Landing improperly from a jump or during sudden direction changes.
Prevention:
- Add balance and proprioception exercises to enhance joint perception.
- Strengthen peroneal and foot stabilizing muscles.
- Utilize ankle bracing or taping in high-risk activities.
- Make sure training and play surfaces are even and well-maintained.
Benefits of Treatment:
- R.I.C.E (Rest, Ice, Compression, Elevation) regimen minimizes acute inflammation.
- Early mobilization and physiotherapy enhance ligament healing and limit stiffness.
- Grade III tears can be treated with PRP, prolotherapy, or surgery in chronic instability.
- Long-term rehab maintains joint function and lessens recurrence.
- Return to sport is generally 2–12 weeks depending on the grade of injury and treatment strategy.
Treatment Option:
- Lateral Ligament Reconstruction (Broström Procedure): Tightening or reconstructing torn ATFL and CFL ligaments for chronic instability.
- Allograft Reconstruction: In revision or complex ligament injuries.
